(Peer-Reviewed) Inactivated SARS-CoV-2 vaccine does not influence the profile of prothrombotic antibody nor increase the risk of thrombosis in a prospective Chinese cohort
Tingting Liu 刘婷婷 ¹, Jing Dai ², Zhitao Yang 杨志涛 ³, Xiaoqi Yu ⁴, Yanping Xu ⁵ ⁶ ⁷, Xinming Shi ², Dong Wei ⁴, Zihan Tang ¹, Guanqun Xu 徐冠群 ², Wenxin Xu ⁴, Yu Liu ², Ce Shi ², Qi Ni 倪琪 ², Chengde Yang 杨程德 ¹, Xinxin Zhang 张欣欣 ⁴, Xuefeng Wang 王学锋 ², Erzhen Chen 陈尔真 ³, Jieming Qu 瞿介明 ⁵ ⁶ ⁷
¹ Department of Rheumatology and Immunology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院附属瑞金医院 风湿免疫科
² Department of Laboratory Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院附属瑞金医院 检验科
³ Department of Emergency, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院附属瑞金医院 急诊科
⁴ Department of Infectious Diseases, Research Laboratory of Clinical Virology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院附属瑞金医院 感染科 临床病毒学研究室
⁵ Department of Pulmonary and Critical Care Medicine, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院附属瑞金医院 呼吸与危重症医学科
⁶ Institute of Respiratory Diseases, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 上海交通大学医学院 呼吸疾病研究所
⁷ Shanghai Key Laboratory of Emergency Prevention, Diagnosis and Treatment of Respiratory Infectious Diseases, Shanghai 200025, China
Science Bulletin, 2021-07-27
Abstract
The presence of antiphospholipid antibodies was shown to be associated with thrombosis in coronavirus disease 2019 (COVID-19) patients. Recently, according to reports from several studies, the vaccine-induced immune thrombotic thrombocytopenia is mediated by anti-platelet factor 4 (PF4)-polyanion complex in adenovirus-vectored COVID-19 vaccine recipients. It is impendent to explore whether inactivated COVID-19 vaccine widely used in China influences prothrombotic autoantibody production and induces thrombosis.
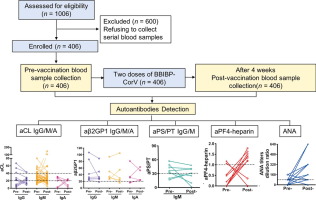
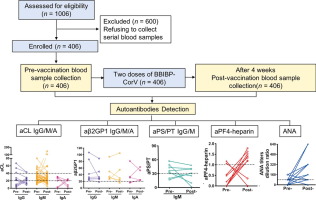
In this prospective study, we recruited 406 healthcare workers who received two doses, 21 days apart, of inactivated severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine (BBIBP-CorV, Sinopharm). Paired blood samples taken before vaccination and four weeks after the second vaccination were used in detecting prothrombotic autoantibodies, including anticardiolipin (aCL), anti-β2 glycoprotein I (aβ2GP1), anti-phosphatidylserine/prothrombin (aPS/PT), and anti-PF4-heparin.
The seroconversion rate of SARS-CoV-2 specific antibodies was 95.81% (389/406) four weeks after vaccination. None of the subjects had spontaneous thrombosis or thrombocytopenia over a minimum follow-up period of eight weeks. There was no significant difference in the presence of all ten autoantibodies between samples collected before and after vaccination: for aCL, IgG (7 vs. 8, P = 0.76), IgM (41 vs. 44, P = 0.73), IgA (4 vs. 4, P = 1.00); anti-β2GP1, IgG (7 vs. 6, P = 0.78), IgM (6 vs. 5, P = 0.76), IgA (3 vs. 5, P = 0.72); aPS/PT IgG (0 vs. 0, P = 1.00), IgM (6 vs. 5, P = 0.76); aPF4-heparin (2 vs. 7, P = 0.18), and antinuclear antibody (ANA) (18 vs. 21, P = 0.62).
Notably, seven cases presented with anti-PF4-heparin antibodies (range: 1.18–1.79 U/mL) after vaccination, and none of them exhibited any sign of thrombotic disorder. In conclusion, inactivated SARS-CoV-2 vaccine does not influence the profile of antiphospholipid antibody and anti-PF4-heparin antibody nor increase the risk of thrombosis.
Separation and identification of mixed signal for distributed acoustic sensor using deep learning
Huaxin Gu, Jingming Zhang, Xingwei Chen, Feihong Yu, Deyu Xu, Shuaiqi Liu, Weihao Lin, Xiaobing Shi, Zixing Huang, Xiongji Yang, Qingchang Hu, Liyang Shao
Opto-Electronic Advances
2025-11-25
A review on optical torques: from engineered light fields to objects
Tao He, Jingyao Zhang, Din Ping Tsai, Junxiao Zhou, Haiyang Huang, Weicheng Yi, Zeyong Wei Yan Zu, Qinghua Song, Zhanshan Wang, Cheng-Wei Qiu, Yuzhi Shi, Xinbin Cheng
Opto-Electronic Science
2025-11-25