(Peer-Reviewed) Peripancreatic vascular involvement in patients with type 1 autoimmune pancreatitis
Meizi Li ¹, Xiaoyin Bai ¹, Kai Xu 徐凯 ², Xi Wu 吴晰 ¹, Tao Guo 郭涛 ¹, Qingwei Jiang 蒋青伟 ¹, Qiang Wang 王强 ¹, Shengyu Zhang ¹, Yingyun Yang ¹, Yunlu Feng 冯云路 ¹, Aiming Yang 杨爱明 ¹
¹ Department of Gastroenterology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Peking Union Medical College and Chinese Academy of Medical Sciences, Beijing, China
中国 北京 中国医学科学院 北京协和医学院 北京协和医院消化内科 疑难重症及罕见病国家重点实验室
² Department of Radiology, Peking Union Medical College Hospital, Beijing, China
中国 北京 北京协和医院放射科
Hepatobiliary Surgery and Nutrition, 2021-05-13
Background
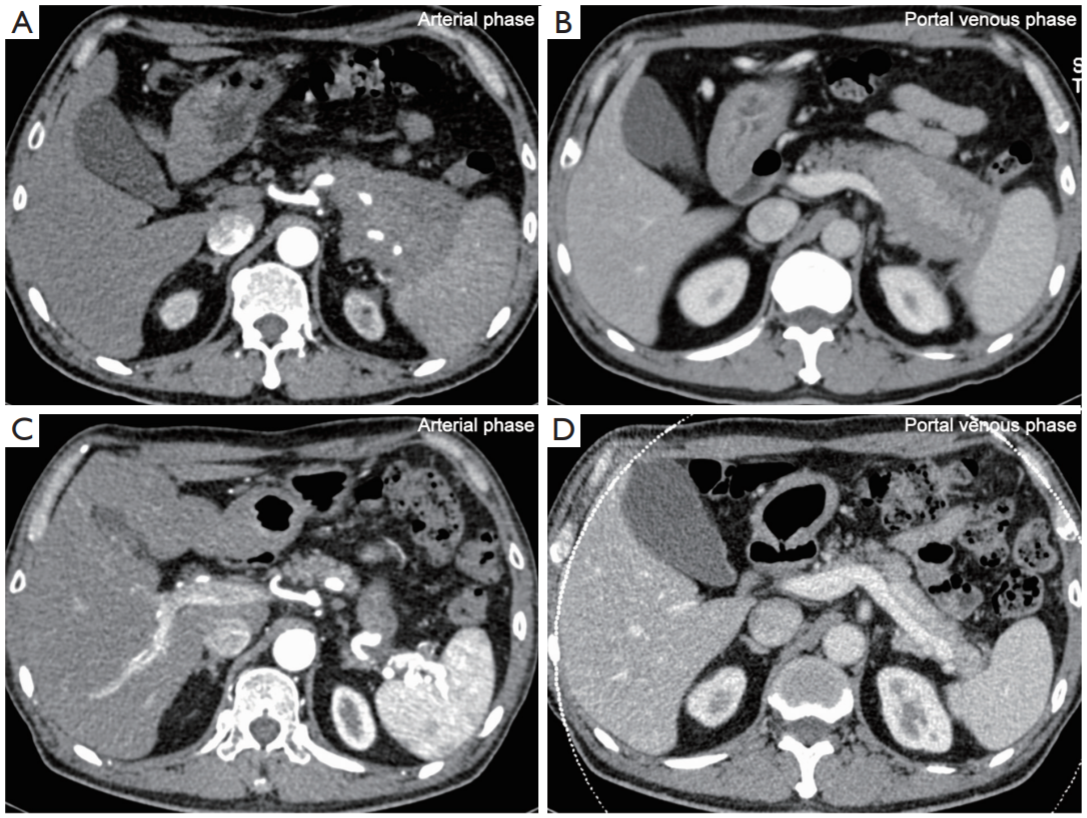
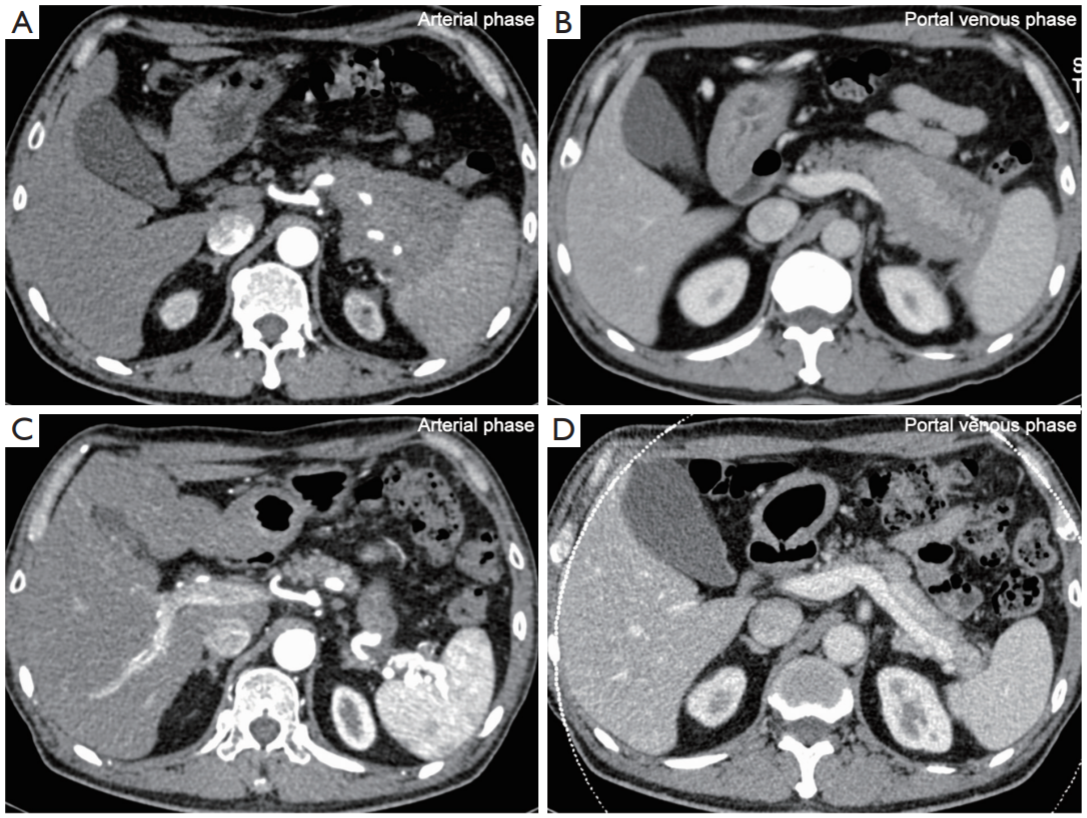
Type 1 autoimmune pancreatitis (AIP) is the pancreatic manifestation of IgG4-related disease. However, this benign disease can result in the peripancreatic vascular involvement (PVI) on occasion, which increases the difficulty of diagnosis and treatment of this clinical entity as well as for differentiating it from pancreatic malignancies.
Methods
We retrospectively reviewed the information on demographics, clinical presentation, laboratory, imaging and endoscopic findings of 101 hospitalized patients with type 1 AIP treated in our department. All the patients were divided into non-PVI and PVI groups according to the first hospitalized medical data. Univariate and multivariate analyses were performed to analyse the potential predictive parameter(s) of PVI in AIP patients.
Results
Among the 101 type 1 AIP patients, 52 (51.5%) exhibited PVI, with a male/female ratio 5.5:1. Their average age was 58.37±8.68 years old. Univariate analysis revealed that the location of pancreatitis lesions, including the pancreatic tail (P=0.010), the presence of splenomegaly (P=0.001) and the white blood cell (WBC) number in peripheral blood (P=0.020), were significantly associated with PVI. The location of pancreatitis lesions, including the pancreatic tail (P=0.023), and the presence of splenomegaly (P=0.010) were found to be independent predictors of the development of PVI by a multivariable regression analysis. A total of 18 out of 25 patients in PVI group who underwent corticosteroid treatment and no less than 6 months radiological follow-up showed improvement in vascular lesions, and no case exhibited exacerbation of PVI lesions during follow-up. Of 36 patients in non-PVI group who were followed up for no less than 6 months, only one case exhibited PVI.
Conclusions
This retrospective study demonstrated that type 1 AIP was associated with a high proportion of PVI. Pancreatic tail involvement and splenomegaly may predict the PVI in type 1 AIP. PVI lesions are reversible in a subset of patients.
Separation and identification of mixed signal for distributed acoustic sensor using deep learning
Huaxin Gu, Jingming Zhang, Xingwei Chen, Feihong Yu, Deyu Xu, Shuaiqi Liu, Weihao Lin, Xiaobing Shi, Zixing Huang, Xiongji Yang, Qingchang Hu, Liyang Shao
Opto-Electronic Advances
2025-11-25